" Nivarak Health Care " Diagnostic Center
Cardiac Ultrasound
Indications
- Assessment of the presence of pericardial effusion
- Assessment of global cardiac systolic function
- Identification of marked RV/LV enlargement
- Intravascular volume status
- Guidance of pericardiocentesis
- Confirmation of transvenous pacing wire placement
Key Ultrasound Anatomy
Documentation
Cardiac ultrasound should include representative image or clip from each of the following windows:
- Subxiphoid/Subcostal
- Parasternal Long Axis
- Parasternal Short Axis
- Apical
Approach
A cardiac for pericardial effusion and cardiac function/activity should include adequate views of the heart including anterior and posterior pericardium and should include the following windows: Subxiphoid/Subcostal, Parasternal Long Axis, Parasternal Short Axis, Apical
Probe and Positioning
- 2-5 MHz curvilinear abdominal probe or smaller footprint curved array or phased array probe
- Patient is supine or in left lateral decubitus position.
Basic Anatomy
Basic Anatomy; From Introduction to Bedside Ultrasound
Soft Tissue
Soft tissue layers can be divided into superficial and deep portions. The superficial portion consists of the epidermis/dermis and the subcutaneous tissue. The epidermis/dermis will appear as a solid hyperechoic line of varying thickness at the very top of the screen. The subcutaneous tissue is relatively hypoechoic with intermittent lace like stranding. The deep portion consists of muscles, tendons, ligaments, bones and joint spaces. Notice that the muscular fascia, which is a hyperechoic line, separates the superficial from deep portion. Nerves and blood vessels will often run in this area. Muscle appears hyperechoic relative to subcutaneous tissue with striations that run parallel in a particular direction. At the bottom of the image we appreciate bone which is a smooth hyperechoic line with posterior shadowing given its strong reflector properties.
Tendon
Tendons will share a similar fibrillar appearance to muscle however given that they are more dense, they will appear more hyperechoic relatively. This is appreciated in the longitudinal view of the supraspinatus tendon seen to the left.
Transverse View of Median Nerve.
Nerve
Nerves take on a unique appearance on ultrasound. Specifically in a transverse plane, their pattern can be described as a honeycomb, which is a direct result of alternating hypoechoic axonal areas and hyperechoic peri-/epineurium, Note the honeycomb appearance in the transverse image of the median nerve seen to the left.
Basic Concepts
Probe: The majority of the time you will be using a high-frequency linear probe. This is ideal since most structures will be superficial and you will want high resolution for proper tissue differentiation. You may decide to use the curvilinear probe when evaluating the hip or performing a nerve block in a larger person.
Positioning: This will vary quite significantly depending on what you are scanning. The key is to make sure the patient is in a comfortable position and that you are supporting the extremity you are examining to avoid unnecessary movement and artifact.
Orientation: You may find yourself on the left side of the patient, at the head of the bed, or even at the patient's backside. Regardless of the patient, be sure to keep your probe marker on the same side relative to yourself so you never confuse yourself with orientation. The area of interest can then be systematically assessed in two orthogonal planes.
Compare: Remember that your patients have two of everything. While you may not initially be certain about potential pathology you see, it is helpful to compare your examination to the contralateral side to help with deciding normal versus abnormal.
Dynamic imaging: Musculoskeletal ultrasound should be interactive, allowing you to assess function and procedure efficacy in real time. For example, when assessing for tendon injury you should be ranging the extremity while observing for tendon abnormalities, or monitoring your needle advance into a fracture site for a hematoma block.
Water bath for small part evaluation; From Introduction to Bedside Ultrasound
Small part imaging:
You may find it difficult to assess a finger tendon or small joint given the size of the body part, the superficial nature of the structure of interest, or even patient discomfort. The water bath will be your best friend here and will allow for excellent visualization of your anatomy as well as less pain for the patient. You may also try a plentiful quantity of gel, however this can get messy.
Anisotropy:
This is a key concept to understand in MSK ultrasound. Anisotropy translates to mean "directionally dependent" and is a result of the fibrillar nature of structures such as tendons and nerves (and to a lesser extent muscle). This quality leads to the ultrasound image varying depending on the angle between the structure of interest and the ultrasound beam (also known as the angle of insonation). For example, when the angle of insonation is perpendicular to a tendon, the tendon appear bright and normal, however as the angle varies, the tendon can take on a hypoechoic appearance. Do not be fooled by this when evaluating for a tear, as you may just be appreciating this phenomenon. However if you do notice that a muscle or tendon does not display the property of anisotropy, this can be a sign of underlying muscle or tendon pathology. For a quick video explanation of this phenomenon.
Lung Ultrasound Introduction & Basic Applications
Performing Ultrasound of the lungs was initially thought to be impossible given air is the enemy . This changed in 1995 when Lichtenstein published an approach to imaging pneumothorax with US. Since then, analyzing artifacts produced by the normal and pathologic lung has become central to diagnostic lung ultrasound.
Indications
Established/great evidence
- The critically ill patient presenting with dyspnea
- Pneumothorax (PTX)
- Pleural effusions
- Acute Decompensated Heart Failure (ADHF)
Developing/emerging literature
- ARDS vs ADHF
- Consolidation/PNA
- Airway management
- Neonatal
A-lines
- An artifact of normal lung, best visualized in hyperinflated lungs (COPD) given more air, or extrapleural free air (PTX)
- Best produced by free air, but well produced by aerated lungs, generally absent in interstitial syndromes, consolidations or effusions
- Horizontal hyperechoic lines projecting at regular intervals throughout the depth of the screen
- These lines represent the pleural line
B-lines (aka comet tails)
- Discrete, laser-like, vertical hyperechoic reverberation artifacts that arise from the pleural line, extend to the bottom of the screen without fading and move synchronously with lung sliding and ventilation
- Erase A-lines
- Occur in interstitial states where there is extra-alveolar fluid collection (ADHF)
- Some ( less than 3) B-lines can be present in normal, non fluid-overloaded lungs
- Produced by reverberation of the sound waves in between air filled alveoli and fluid filled interstitium
Probe Selection & Positioning
- No consensus on the best probe to use
- High frequency linear probe good for PTX evaluation
- Lower frequency curvilinear or phased array necessary for deeper evaluation of B-lines, consolidations, pleural effusions
- Curvilinear or phased array probes better for the evaluation of dyspnea in acute patients given the use of one probe increases efficiency of exam
- Less image processing is better given lung US makes use of artifacts
- Turn off filters, high frame per second
- Image processing generally decreases unwanted artifacts which is desirable .
- Patients should be placed supine for the majority of the lung exam
- Extrapleural air will move anteriorly
- Extrapleural fluid will move posteriorly
Pneumothorax (PTX)
- Patient supine, start with transducer oriented vertically on anterior chest wall
- Locate 2 ribs so that the pleural line can be identified correctly
- Once you find lung sliding indicating the pleural line rotate the probe horizontally and then slide within the rib space to assure there is no area lacking lung sliding
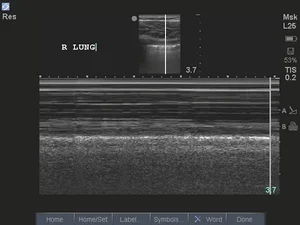
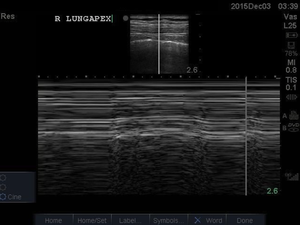
- You can confirm lung sliding with M-Mode and you should visualize the “seashore sign” as above
- The “sand” of the “seashore sign” is produced by haphazard reflection of the sound waves in multiple different directions off of the spherical alveoli
- Air should accumulate most anteriorly in the supine patient so it should be adequate to image just the anterior chest
- If an area of no lung sliding is found, you can use M-mode to confirm which will not show the typical “seashore sign” but will show the “stratosphere sign”
- Pathognomonic for a PTX is the which shows the point at which the lung loses contact with the chest wall
- Lichtenstein’s 1995 article found sensitivity of US of the anterior chest wall to be 95.3% sensitive and 91.1% specific for PTX with a NPV of 100%
- Since then multiple studies have shown superiority of POCUS in ruling out PTX
Pleural effusions
- Patient in a supine position
- Gravity dependent, should flow to the most dependent regions of the pleural cavity
- Image the postero-inferior aspect of the thorax as this is where fluid will accumulate
- The optimal place to visualize a non-loculated pleural effusion is the posterior axillary line just superior to the diaphragm
- M-mode can help differentiate small effusions from pleural thickening if you visualize the sinusoid-sign (swinging of the lung to and fro in the fluid)
- More sensitive than CXR and as sensitive as CT
Pearls and Pitfalls
- Failing to properly identify the pleural line
- Soft tissues and muscles are frequently mistaken for the pleural line if the patient is hyperventilating
- In a tachypneic trauma patient, this can easily be called a false negative for PTX
- Subcutaneous emphysema
- Not suspecting a pulmonary embolus (PE) with a normal lung exam
- Normal lungs are typical of patients with PEs
- Not thinking about performing lung US or thinking it will take too long.
Ultrasound Physics & Knobology
More terminology: Make sure you know how to describe what your seeing.
- Near field: Half of US screen closest your probe.
- Far field: Half of US screen farthest from your probe.
- Hyperechoic: Appears bright and white which means that it contains high calcium content such as bone/stones/tendons.
- Anechoic: Appears black on screen which means it is fluid or artifact known as shadowing
- Grey areas: The inbetween. Describe these areas with respect to surrounding tissue
- Near field: screen closest your probe.
- Far field: screen farthest from your probe.
- Hyperechoic: Appears bright and white which means that it contains high calcium content such as bone/stones/tendons.
- Anechoic: Appears black on screen which means it is fluid or artifact known as shadowing
- Grey areas: The inbetween. Describe these areas with respect to surrounding tissue
Knobology
The art of turning knobs. There are several knobs that we need to know how to use to make our images look better but first a quick look at probe terminology.



































Comments
Post a Comment